Thursday, November 25, 2010
Pallimed Case Conferences (cases.pallimed.org) is closed to comments and new posts as of April 25, 2013.
This site will stay online as an archived source, but will no longer be updated.
For active posts on these cases and new cases go to www.pallimed.com.
For three years running now, many of us bloggers have participated in what we’ve called a “blog rally” to promote Engage With Grace – a movement aimed at making sure all of us understand, communicate, and have honored our end-of-life wishes.
The rally is timed to coincide with a weekend when most of us are with the very people with whom we should be having these unbelievably important conversations – our closest friends and family.
At the heart of Engage With Grace are five questions designed to get the conversation about end-of-life started. We’ve included them at the end of this post. They’re not easy questions, but they are important -- and believe it or not, most people find they actually enjoy discussing their answers with loved ones. The key is having the conversation before it’s too late.
This past year has done so much to support our mission to get more and more people talking about their end-of-life wishes. We’ve heard stories with happy endings … and stories with endings that could’ve (and should’ve) been better. We’ve stared down political opposition. We’ve supported each other’s efforts. And we’ve helped make this a topic of national importance.
So in the spirit of the upcoming Thanksgiving weekend, we’d like to highlight some things for which we’re grateful.
Thank you to Atul Gawande for writing such a fiercely intelligent and compelling piece on “letting go”– it is a work of art, and a must read.
Thank you to whomever perpetuated the myth of “death panels” for putting a fine point on all the things we don’t stand for, and in the process, shining a light on the right we all have to live our lives with intent – right through to the end.
Thank you to TEDMED for letting us share our story and our vision.
And of course, thank you to everyone who has taken this topic so seriously, and to all who have done so much to spread the word, including sharing The One Slide.
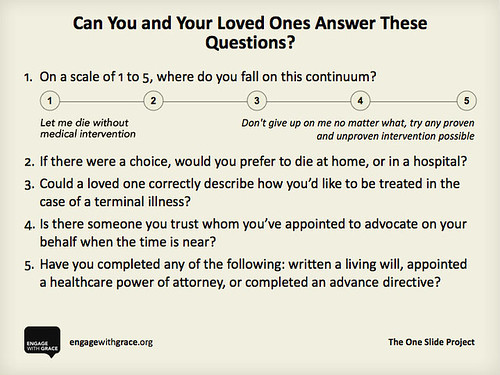
We share our thanks with you, and we ask that you share this slide with your family, friends, and followers. Know the answers for yourself, know the answers for your loved ones, and appoint an advocate who can make sure those wishes get honored – it’s something we think you’ll be thankful for when it matters most.
Here’s to a holiday filled with joy – and as we engage in conversation with the ones we love, we engage with grace.
To learn more please go to www.engagewithgrace.org. This post was written by Alexandra Drane and the Engage With Grace team.
Thursday, November 25, 2010 by Christian Sinclair ·
Thursday, June 17, 2010
Pallimed Case Conferences (cases.pallimed.org) is closed to comments and new posts as of April 25, 2013.
This site will stay online as an archived source, but will no longer be updated.
For active posts on these cases and new cases go to www.pallimed.com.
By Julie Childers, MD
Originally posted at the Institute to Enhance Palliative Care, University of Pittsburgh Medical Center
Vol 10, No. 6 - June 2010
Case: Mrs. L was a 95 year old woman who was admitted to the acute care hospital from her nursing home with decreased mental status. She was found to have pneumonia, and though her infection improved with antibiotics, her mental status did not recover and she continued to be only slightly responsive to her family, unable to eat or interact On the sixth day of Mrs. L’s hospitalization, palliative medicine was consulted to help the family with decision-making. By the time the palliative care consultant saw the patient, a temporary feeding tube had been placed, and the family had reached consensus on a trial of artificial feeding to give her a chance to regain strength, though they acknowledged that her prognosis was poor.
The next day, the patient was still unable to communicate, but was moaning and grimacing. She repeatedly tried to cough weakly to clear the copious secretions in her upper airway. The palliative care consultant recommended low doses of intravenous morphine to treat pain and shortness of breath, with a medication to clear secretions. However, Mrs. L’s attending physician was concerned that treating pain with opioids would cause respiratory depression and lead to Mrs. L’s death. The next night, the bedside nurse charted several times that Mrs. L was screaming, but they were only able to give her Tylenol for pain; she required wrist restraints to prevent her from pulling out her feeding tube. The palliative care physician was haunted by the image of the dying 95 year old woman, tied down and denied treatment for her suffering.
Discussion: Moral distress occurs when the clinician knows the appropriate action to take, but is unable to carry it out, and feels forced to give care contrary to her values. It is more often described in the nursing literature, but is beginning to come to the awareness of physicians as well. Moral distress often occurs in end-of-life situations when the decision is made to provide aggressive life-sustaining treatments that are felt to put excessive burden on patients and families.
Clinicians who see patients at the end of life may be particularly vulnerable to moral distress. For those of us who serve as consultants, our involvement in a case is at the discretion of the attending physician. In cases such as Mrs. L’s, we feel constrained by our role as advisors to the consulting physicians and the expectation of professional courtesy towards other physicians’ decisions. When we serve as attending physicians ourselves, our ability to relieve patient suffering may be limited by the family’s preference that every possible life-sustaining measure be taken.
Moral distress is also a common problem in the nursing field, particularly critical care nursing. For clinicians in any of these roles, moral distress arises when the system or other people interfere with our ability to relieve a dying patient’s suffering.
In the nursing literature, moral distress has been shown to contribute to decreased job satisfaction and to burnout. The American Academy of Critical Care Nurses recommends addressing moral distress with a four-step process:
- Ask: You may not even be aware that you are suffering from moral distress. Signs of moral distress may include physical illnesses, poor sleep, and fatigue; addictive behaviors; disconnection with family or community; and either over-involvement or disengagement from patients and families.
- Affirm: Validate the distress by discussing these feelings and perceptions with others. Make a commitment to caring for yourself by addressing moral distress.
- Assess: Identify sources of your distress, and rate its severity. Determine your readiness to act, and what impact your action would have on professional relationships, patients, and families.
- Act: Identify appropriate sources of support, reduce the risks of taking action when possible, and maximize your strengths. Then you may decide to act to address a specific source of distress in your work environment.
In Mrs. L’s case, the consultant discussed the case with the interdisciplinary team, receiving support for her concerns. Despite fear of negative repercussions from the primary service, she called the patient’s son herself and gently explained the signs of suffering that Mrs. L was showing. He agreed that his mother should have low-dose morphine. The primary team added this order without any expressed objections to the consultant stepping over her boundaries. Mrs. L died a few days later.
References
1. Weissman, D. Moral distress in palliative care. Journal of Palliative Medicine. October 2009, 12(10): 865-866.
2. The American Association of Critical Care Nurses. The 4 A’s for managing moral distress. (free pdf)
Thursday, June 17, 2010 by Christian Sinclair ·
Subscribe to:
Comments (Atom)


